Some patients, who are going to get a dental implant, face a problem when they consult their doctor: there is not enough jawbone for an implant. Additionally, the implantologist scares you with a dreadful surgery to build up bone tissue or offers you to give up a beautiful, healthy smile altogether. In this article, you will learn what bone grafting is and whether it is so frightful.
Bone grafting is a surgical procedure to restore jawbone volume for subsequent implant placement. There are different types of bone graft: dry powder bone and live bone. We do not recommend using dry bone because the healing process will take much longer. We use live bone from the bank of tissues, which takes root very well.
When is osteoplastic surgery recommended?
- The patient needs an implant in an area where a tooth was extracted several years (or months) ago.
- The patient has anatomically large maxillary sinuses or physiologically small bone volume.
- There are inflammations in the patient’s mouth (cysts, granulomas, periodontitis) that contribute to bone resorption.
- Extraction of a tooth with the root — osteoplastic surgery — is performed in order to preserve the volume of the jaw tissue.
What is bone grafting?
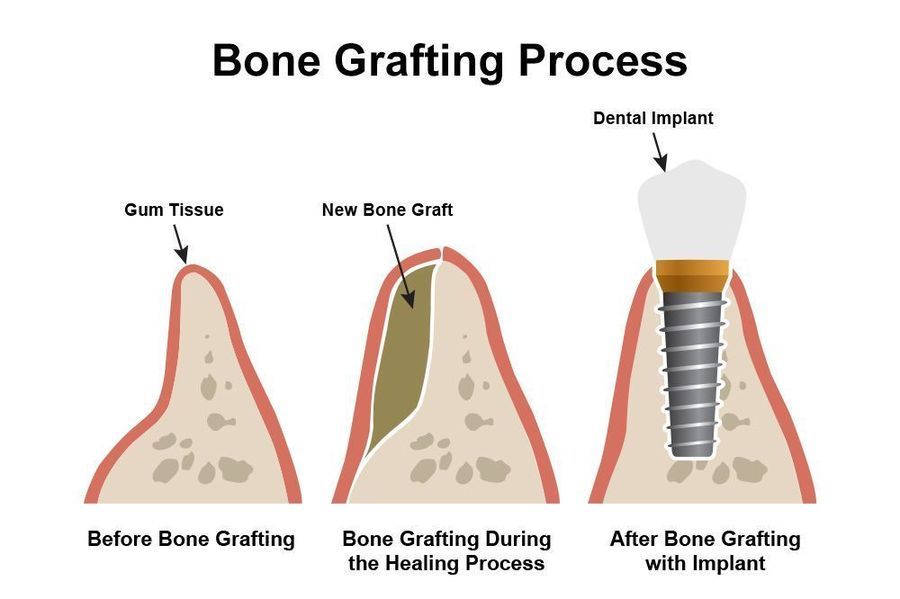
A bone graft is immediately placed in the open wound after extraction. The tissues are treated so that the material stays inside. The grafting process takes about 8 weeks. Then, the patient visits the clinic to have the doctor take an X-ray and to make sure the exposed area is ready for the implant.
What are the consequences if a tooth extraction area is left empty?


In our practice, we see numerous cases where patients, who have had a tooth extracted, do not have bone augmentation or an implant placed, but simply leave an empty space. The bone around the defect begins to resorb after some time. As a result, the adjacent teeth are gradually shifted in the direction of the defect, the bite is disturbed, and there are problems when chewing food. Now, instead of one tooth, you have to restore 2–3 or more, which is much more expensive.
Is bone grafting really necessary?
One-stage implantation with instant loading, when the placement of implants and fixation of a temporary prosthesis are carried out simultaneously with the removal of the affected teeth, allows you to return all of your teeth without bone grafting.
With the loss of all teeth and mild/moderate loss of bone, the teeth are restored with All-on-four/All-on-six without osteoplastic surgery. A distinctive feature of these methods is that the implants are placed at a 35-degree angle in the distal sections, which requires much less jawbone. Single defects are restored with short, narrow implants, with minimal bone loss.
Doctors recommend Nobel Zygoma implants for patients with total adentia and critical bone volume on the upper jaw. The method involves implanting 4 or 6 artificial roots into the zygomatic bone, which is not subject to atrophy. Thanks to this, the patient receives a fixed prosthesis without osteoplastic surgery.
The best materials for bone grafting
The peculiarity of modern materials used in osteoplastic surgery is osteoconduction — the ability of the artificial bone to resorb when the natural bone grows. Today, there are four types of grafts:
- Autografts
Natural bone (autologous bone) taken from extraoral or intraoral areas. Suitable for osteoplastic surgery. Has a high survival rate and excellent biocompatibility. Requires additional intervention to take bone from another part of the patient’s body. - Alloplastic grafts
A synthetic bone powder that stimulates bone regeneration. Biocompatible with mineralized tissues. May cause an allergic reaction. - Xenografts
A bone block from cattle. The material is processed to increase its biocompatibility after harvesting. - Allografts
Human donor bone. In contrast to autografts, the use of allografts does not require an additional bone harvesting. The surgery is less traumatic. To exclude the transmission of infectious diseases, the allograft is treated and sterilized during harvesting. The material has high biocompatibility.
At Svetlana Dental, we use live bone from a bank. This approach allows you to build up bone tissue with minimal trauma to the patient, ensures high engraftment of osteogenic material, and excludes the development of allergies and complications. Each bone graft sample is checked for diseases (HIV, AIDS, hepatitis, syphilis, etc.) and has its document and an individual serial number.
 When can you have osteoplastic surgery?
When can you have osteoplastic surgery?
A fairly large number of patients are in no hurry to solve the problem of replacing the lost unit after tooth extraction. As a result of prolonged dental absence, atrophy of the jaw tissue develops — a direct contraindication for the placement of implants. Therefore, before implants are placed, the patient often needs to build up the amount of bone to securely attach the titanium posts.
Modern dentistry allows you to build up bone in conjunction with tooth extraction and, in some cases, you can immediately install a dental implant, provided that the mouth is free of inflammation.
Methods of bone augmentation
Depending on the clinical picture, the bone volume is restored in different ways:
 Sinus lift
Sinus lift
Osteoplastic surgery aimed at bone regeneration exclusively on the upper jaw in the area of the maxillary sinus. Performed before or together with implantation. Indicated when there is a risk of damage or piercing of the maxillary sinus floor with an implant.
The process of surgery:
- The doctor peels off the mucous membrane from the lower wall (bottom) of the sinus and lifts it up.
- Places the bone material on the lower wall, covers it with a barrier membrane and mucosal flaps, and then sutures the tissues.
There are two types of sinus lift:
- Closed — a minimally invasive method where the doctor builds up the volume of bone directly through the seat, then plants a dental implant. Indicated for the bone volume of 5 mm or more.
- Open — a difficult and traumatic, but predictable method of osteoplastic surgery. Indicated in cases of significant bone atrophy.
Splitting of the dental arch
Recommended for those with insufficient alveolar ridge thickness for implants in any jaw. The surgery requires dense bone walls at least 2.5 mm thick and 12 mm high.
The process of surgery:
- The doctor cuts the ridge of the bone horizontally.
- Extends its edges to the size necessary to place the implant.
- Screws a titanium rod into the gap.
- The free space around it is filled with donor or artificial bone.
- Sutures the gum and covers it with a barrier membrane on top.
The surgery is usually performed using the Split-Control technology, which allows an artificial root to be implanted in conjunction with bone augmentation. After 3–6 months, the implant is loaded with a permanent prosthesis.
Guided tissue regeneration
The method is used for minor or moderate bone loss. The procedure is performed in conjunction with the implantation.
The process of surgery:
- The doctor fills the defect with a bone graft and places an implant.
- Applies a barrier and a platelet-rich fibrin membrane (PRF) to the area. The first membrane relieves tissue pressure on the defect and protects it from adverse effects. The second membrane, rich in platelets, helps tissues recover faster, which shortens the rehabilitation period.
 Bone block transplantation
Bone block transplantation
The method involves the transplantation of an autograft. Recommended for patients whose bodies do not accept transplants other than autogenous bone. Allows to increase the dental arch in height and width. The implant is placed only after the bone is completely healed. The surgery consists of two steps: the harvesting and transplantation of donor bone to the area where the implant is placed:
- After preparing the autograft, the surgeon fixes it with titanium screws in the area of the defect.
- Then covers it with a membrane and sutures the area.
Full bone regeneration takes 2–3 months, then you can put an implant. Titanium screws are removed just before dental implants are placed. To avoid recurrent bone atrophy due to lack of load, implants must be placed immediately after tissue healing.
Stages of the procedure
Regardless of the method of osteoplastic surgery, bone augmentation consists of three steps:
- Anesthesia: The patient is put under medical sedation for the procedure to be painless.
- Osteoplastic surgery: Bone volume is increased by the selected method. The deficit area is filled with a bone graft and covered with a membrane.
- Implantation: Dental implants are placed simultaneously with bone grafting if the clinical case allows. Otherwise, the gum is sutured and implantation is performed after full tissue regeneration, 3–6 months later.
Rehabilitation process
Osteoplastic surgery is a procedure involving trauma to the tissues of the mouth. Pain and discomfort are normal postoperative phenomena.
First days after surgery
Follow these recommendations so that the postoperative rehabilitation will go without complications:
- During the first 2 hours after the procedure, apply a cold compress to the operated area (for 5 minutes at intervals of 15 minutes).
- Take medication prescribed by your doctor.
- Exclude physical activities.
- Do not eat hot, spicy, hard, or salty foods.
- For the first 3–4 days, do mouth baths and avoid vigorous mouthwash.
- Brush your teeth with a soft toothbrush 2–3 days after the procedure.
- Clean the sutures periodically. Treat the injured area with a tampon soaked in antiseptic. Apply an ointment to the sutures that will speed up tissue healing (prescribed by your doctor).
One week after surgery
Usually, by this time, the injured tissues have healed, which means you can return to your normal life. Increase physical activity gradually. If the exposed area does not disturb you and sutures are removed, you can carefully add solid foods to the menu and conduct full oral hygiene.
Possible complications
Normal symptoms that may bother you after osteoplastic surgery:
- Swelling of the mucosa of the mouth and face on the healing side: 48–72 hours.
- Body temperature of 38–39 degrees Celsius: up to 72 hours.
- Pain and discharge in the exposed area: up to 72 hours (pain gradually subsides).
- Minor bleeding after the procedure: up to 72 hours.
- Hypersalivation: up to 72 hours.
- Facial hematoma: up to 7 days.
- Partial facial numbness: up to 7 days.
- Runny nose with transparent discharge: up to 14 days.
 Consult a doctor immediately if:
Consult a doctor immediately if:
- The swelling doesn’t go away after 4 days.
- The fever doesn’t go away after 4 days.
- The sutures come apart immediately after surgery or a few days later.
- You have profuse discharge with an unpleasant odor in the exposed area.
- Profuse bleeding lasts 3 hours or more after surgery.
- There is drop-out of bone material or loosening of the dental implant.
- Facial numbness and hypersalivation last more than 7 days.
- Persistent runny nose with exudate from the nose lasts several days.
How painful is the procedure?
The surgeon performs all manipulations under anesthesia. The patient feels no pain or discomfort. After surgery, the doctor prescribes medication to relieve pain and swelling. Ten days after the tooth extraction and bone augmentation, you should come in for a checkup to make sure that the healing process goes without complications.
How much does it cost?
The price depends on the amount of bone used. On average, $500 to $750. This is nothing compared to how much you’ll have to pay if you don’t get your lost tooth fixed. Call our office at 954-457-8308 for more information.